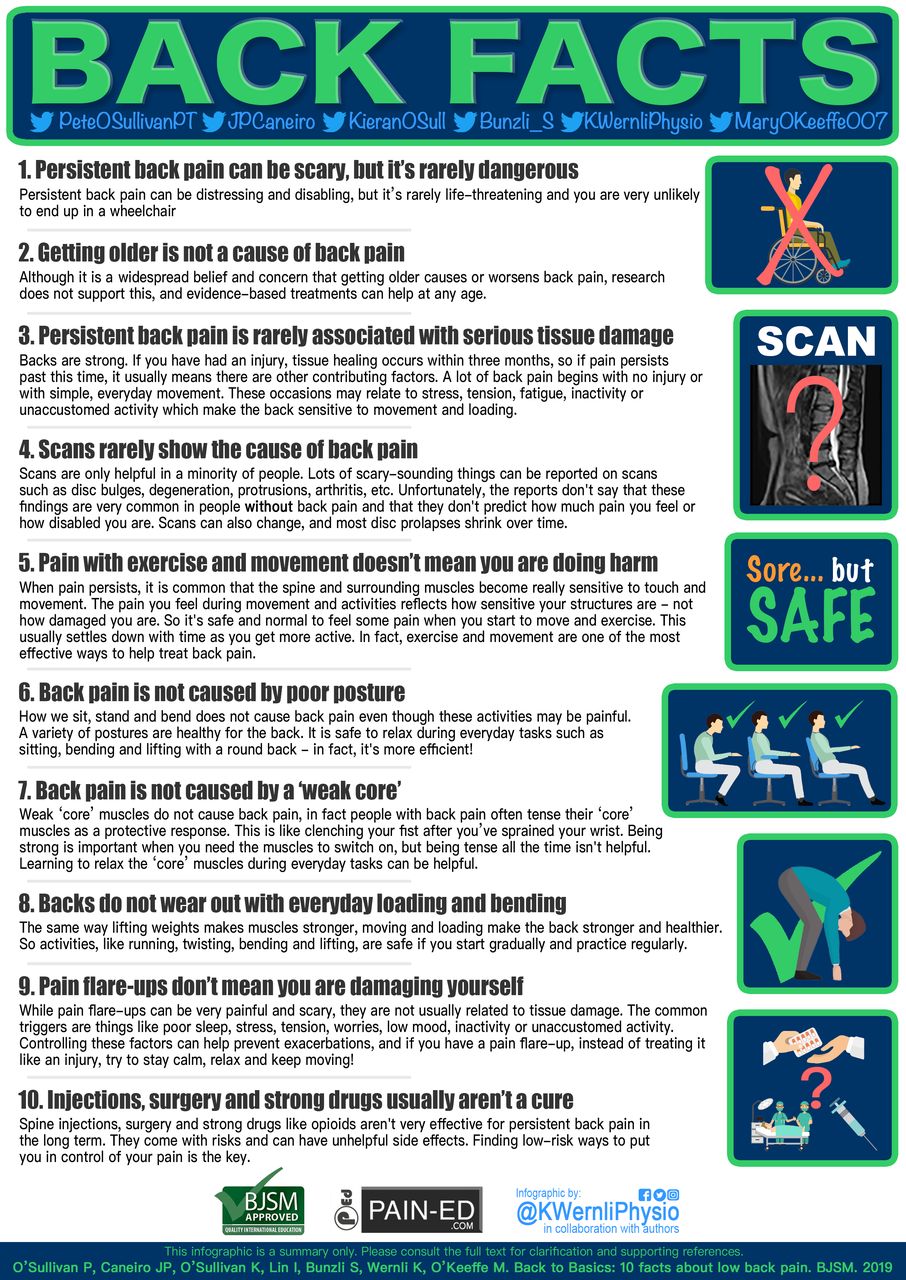
What is Endometriosis?
Endometriosis is a persistent inflammatory medical condition characterized by the endometrial-like tissue growing outside the uterus. These cells are often found in the pelvis (on the thin pelvic lining called the peritoneum), including the ovaries, pelvic ligaments, bowel & the bladder, & they have also been located as far away as the lungs & the brain.
Symptoms can emerge as early as eight years of age & the cause is now generally considered multi-factorial with a strong genetic link, possibly also how genetics behave with other influences (perhaps by environmental factors for example).
In Aotearoa/New Zealand, it affects approximately 1 in 10 women & individuals presumed female at birth in their reproductive years (In Australia 1 in 7) & may take 7-8 years to reach a formal diagnosis. It has been reported that endometriosis patients can be disbelieved or dismissed by their healthcare professionals which in part is due to long diagnostic delays.
Symptoms associated with endometriosis are wide ranging & may include:-
♀️Fatigue
♀️Pain in the pelvic region, lower back or legs
♀️Pain with bowel movements
♀️Heavy bleeding (menorrhagia) or irregular bleeding
♀️Having trouble holding on when you have a full bladder, or having to go frequently
♀️Pain during or after sex (dyspareunia)
♀️Pain when you urinate (dysuria)
♀️Pain on or around ovulation (dysmenorrhea)
♀️Pain that stops you on or around your period
♀️Abdominal bloating, digestive issues
♀️Some women may experience no symptoms.
Symptoms can have significant consequences on various domains of life, including mental health, social & intimate relationships, as well as functioning at school or work. Due to the variation in disease outcomes, there is no one-size-fits-all management approach, & successful management needs to be tailored according to the individual’s presentation & needs.
Endometriosis is more common than diabetes (1 in 20) & cancer (1 in 50) & is one of the most prevalent yet under recognised conditions.
Severity of symptoms may not reflect the extent of the disease, which can cause internal changes without noticeable pain. Sometimes endometriosis can be diagnosed incidentally during medical intervention for other matters.
How is endometriosis treated?
There are three types of treatments for endometriosis:
1. Medical treatments – Includes medications to manage symptoms & hormone therapies.
2. Surgical treatments – Involves procedures such as laparoscopy to remove endometriotic tissue.
3. Allied treatments – research shows multimodal physiotherapy is superior for pain relief & overall well-being than any other modality (e.g. acupuncture).
(Starzec-Proserpio et al, 2024).
How is it diagnosed?
The only definitive way to diagnose endometriosis is through laparoscopy with a biopsy (tissue sample). The tissue can form nodules & plaques which can be visualised here.
There is currently no cure for endometriosis.
Fertility
Endometriosis may impact fertility by causing inflammatory changes within the pelvis making the environment too hostile for the egg, sperm & embryo & thus impact implantation of the embyro.
Research suggests ≈30% undergoing IVF have endometriosis & ≈50% of those living with endometriosis are challenged by fertility.
Early diagnosis & treatment can help stop disease progression & worsening fertility prospects.
Work Impact
Research shows :-
♀️50% of endometriosis sufferers report lack of flexibility in the workplace was a significant problem.
♀️70% of women have to take unpaid time off to manage their endometriosis symptoms.
♀️1 in 3 have been passed over for promotion.
♀️1 in 6 have lost their employment due to their endometriosis.
♀️Many women are fearful of raising the issue in the workplace.
♀️1 in 10 individuals with endometriosis leaving employment due to the overwhelming demands of managing their condition.
Impact of COVID-19 Pandemic
Workplace changes built on flexibility positively impacted those with endometriosis.
79% reported management of their endometriosis symptoms easier.
60% said they were more productive with Work from Home options.
Other tips to improve endometriosis management in the workplace:
- Introduction of 20-minute rest periods
- Access to healthcare benefit
- Access to healthcare services such as counselling, mindfulness or assisted exercise
- Access to physical aids such as ergonomic chairs, heat packs, props.
Some helpful patient reported outcome measures to fill out are:-
- The Endometriosis Impact Questionnaire (EIQ) a comprehensive self-report tool designed to assess the long-term effects of endometriosis on various aspects of women’s lives. It evaluates physical, psychological, social, sexual, occupational, educational & lifestyle impacts.
View EIQ Tool Here - Pelvic Pain Impact Questionnaire (PPIQ)
View PPIQ Questionnaire Here